She likely acquired a bacterial infection while in hospital during one of many complicated facial surgeries. None of the many doctors she had in the first six years of those surgeries ever mentioned antibiotic resistance to her. Because she was oblivious to the dangers of stopping an antibiotic drug or even an antibiotic ointment after a couple days when it appeared to not be working, she sees herself as part of the complication – back then.

Vanessa Carter nearly lost her face to antibiotic resistance
Now, she is a force for common knowledge.
“What should be common knowledge?” the self-described patient advocate begins to explain. What smoking is to cancer, the abuse of antibiotics should be to drug resistance, she continues.
“Taking two doses of an antibiotic in the morning because you might forget at lunch time could aggravate resistance. That should be common knowledge. Double-dosing your child could aggravate resistance. That should be common knowledge.”
Patients need more information, Carter says. “It could have made a massive difference to my face and to my life at that time.”
“Don’t dumb it down,” stresses Carter, who also works feverishly for behaviour change at all levels, from patients to medical practitioners to researchers and private sector marketers. “Teach people so they can empower themselves so they can participate in the management of infections in and out of hospital. I’ve never seen antibiotic packaging that warns a person about resistance. When I go to a pharmacy, I ask for inserts about various antibiotics, and I don’t see it. That would be one avenue to improve communication.”
Carter required an extensive facial reconstruction after a car accident in 2004 in Johannesburg, South Africa, that severely injured her abdomen and face, including a broken nose, a smashed cheekbone and eye socket, loss of her right eye, a broken jaw and massive facial lacerations. She also sustained neck and back injuries as well as a fractured pelvic bone.
She acquired two antibiotic-resistant infections during the decade it took to reconstruct her face. The first occurred in 2010 when bacteria formed on the alloplastic prosthetic inserted under her right eye socket. The infection did not respond to the antibiotics prescribed, and it wasn’t until nearly a year later that it was diagnosed as methicillin-resistant Staphylococcus aureus.
There was no medical team communication about her situation. She heard differing advice from each of her super specialists. Some of them insisted the prosthetic should remain because the infection was elsewhere. Her plastic surgeon went against them and removed it, which likely saved her life.
The infection returned in 2012, along with an allergy, after yet another surgery. The infection could have come from the hospital or resurfaced from the previously infected area but was resistant to the antibiotic. The allergy was potentially from the antibiotic ointment.
“In your mind you think antibiotic ointment will help heal the wound faster. But we don’t get the explanation that this is an antibiotic. And with medicines as well as ointments, we don’t hear take at “equal” intervals, which is important,” Carter explains. People are accustomed to hearing “take three times a day”, but the advice does not emphasize why it must be at set times, which Carter points out is critical to keeping the bacteria (in the case of antibiotics) from building up their strength.
Taking antimicrobials, including antibiotics, any time of day can lead to either overexposing or underexposing the microbes, again, boosting their resistance, she explains.
What is resistance and what are solutions?
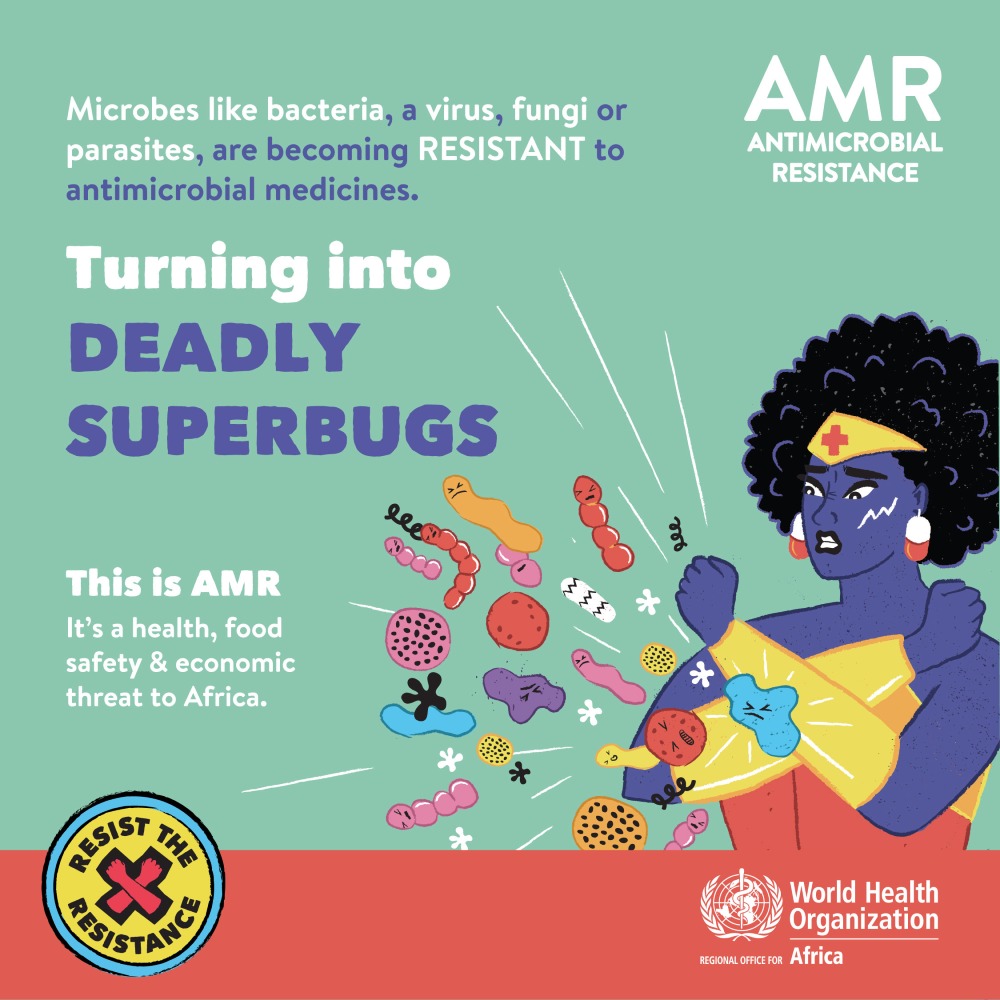
The improper use of antimicrobial medicines, including antibiotics, enables bacteria, viruses, fungi and parasites to mutate into superbugs that are resistant to the drugs designed to kill them.
“Many patients don’t understand that antibiotics are used to treat the dangerous bacteria in their body and not the human body,” says Carter. They think the body becomes resistant to the antibiotic, but it is the bacteria that becomes resistant.
Carter believes pharmaceutical packaging with a warning that misuse of antibiotics can cause bacterial resistance would help counter that confusion.
More conversations about responsible antimicrobial use between patients and all health care workers, including doctors, is a necessity, she stresses.
“Policy is also significant,” she adds. “Why is it so easy to get antibiotics in some countries? And so easy to use them in farming?”
On being a patient advocate
As a patient advocate, Carter spends a great deal of time with academic researchers and advisory groups in South Africa and internationally with ASPIRES, a research collaborative involving Imperial College London, the University of Cape Town and others. With them, the marketing specialist and founder of Healthcare Communications and Social Media South Africa discusses her personal story and views around what could have improved her experience during her many surgeries.
She also works as a “civil society champion” with the African Centres for Disease Control and Prevention, promotes the Antibiotic Guardian pledge campaign in South Africa and has coordinated Twitter chats among leading specialists in the region to amplify awareness on what should be common knowledge about the use of medical drugs, from antibiotics to antimalarials.
Seven years ago, when Carter committed to being a patient advocate, antimicrobial resistance was barely discussed. Conversations have expanded since then, but she sees it as too-slow a pace in what is becoming a race to stymie the increasing resistance of microbes to the drugs available to fight them.
Globally, some 700 000 people die annually because of microbial resistance, according to World Health Organization data. The Review on Antimicrobial Resistance estimates that 4.1 million people in Africa may die of it by 2050 if what should be common practice by patients and medical personnel remains unchanged.
“We live in countries where health care is difficult to access,” she says of the reality that many people in Africa cannot afford to seek out a doctor and sometimes self-medicate with antibiotics or other antimicrobial medicines from unlicensed vendors. “I don’t know if anyone has the answer for how to approach that because, understandably, when you are ill, you do whatever you can to get medication. If it’s difficult to obtain it in the health system, where else do you turn?”
“While I know common knowledge isn’t the silver magic to changing this type of behaviour,” she adds, I believe it is a good place to start.”